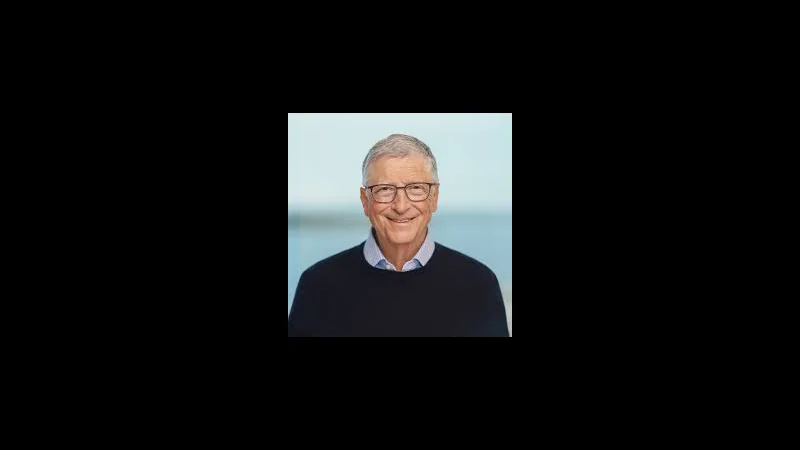
Bill Gates Says AI Will Push Humanity to an Extraordinary Turning Point in Healthcare – What That Really Means

A New “Turning Point” for Global Health
- Anadolu Ajansı
- +1
- Anadolu Ajansı
- +1
- TIME
- +1
- Anadolu Ajansı
- +1
For oracnoos readers, the key question is not whether this is optimistic rhetoric. The deeper question is: what would it take for AI to genuinely change the trajectory of global health – and are we actually on that path?
From Millennium Progress to Fragile Gains
Gates’s remarks are rooted in data compiled over years by the Gates Foundation and groups like the Institute for Health Metrics and Evaluation (IHME). Child deaths have fallen dramatically since 2000 thanks to vaccines, basic primary care, malaria control, and better nutrition.
TIME
- Financial Times
- That increase translates into hundreds of thousands of preventable deaths in a single year.
Against this backdrop, Gates’s “extraordinary turning point” phrase is not a celebration of AI hype. It is a warning: if the world simply keeps doing more of the same – slowly, with shrinking budgets – decades of progress will evaporate. New tools that compress costs and expand reach are needed, and AI is at the top of that list.
Gates’s Healthcare Vision for AI
Gates has been explicit for several years that he sees AI as a technology wave on the scale of the PC, the smartphone, and the internet combined.
gatesnotes.com
Where personal computers put productivity software on every desk, and the internet put information in everyone’s pocket, AI – particularly large language models and domain-specific systems – can put reasoning and expertise in places where professionals simply do not exist today.
At Doha Forum, he emphasized three interlocking themes:
Anadolu Ajansı
+2
Haberler
+2
Primary care in poor countries is drastically under-resourced.
In many regions, one doctor may serve tens of thousands of people, or there may be no doctor at all within a reachable distance.
Most deaths are from conditions that are preventable or treatable.
Gates estimates that with a functional health system and basic interventions, more than 95% of deaths from such conditions in poor countries could be avoided.
Anadolu Ajansı
+1
AI can extend expert-level support to people who currently receive none.
By enabling triage, decision support, and remote consultations in local languages, AI can make low-cost health systems far more capable.
- The argument is not that AI replaces doctors entirely
- but that it can amplify scarce human resources
- create a new tier of “digital primary care
- ” and help health workers at every level make better decisions.
Multilingual AI: Healthcare in Your Own Language
One concrete detail in the Anadolu Ajansı coverage is easy to overlook but strategically critical: Gates highlighted funding for AI models that can understand a wide range of languages and dialects, including those widely spoken across Africa and Asia.
Anadolu Ajansı
+2
Yandex
+2
Why does that matter?
Many communities interact with the health system in local languages that are poorly supported by mainstream AI models.
If AI only works in English or a handful of major languages, it risks deepening inequalities: the people who most need it will be the least able to use it.
- Local-language models can allow patients to describe symptoms
- concerns
- context with nuance – which is central to accurate triage.
- In the Gates vision
- a villager should be able to speak to an AI assistant in their own language
- on a low-end smartphone
- receive:
a first-pass assessment of urgency,
advice on whether to seek immediate in-person care,
clear guidance on warning signs to watch for,
and, where appropriate, a connection to a human clinician via telemedicine.
This is not speculative. Gates has repeatedly pointed out that AI is already capable of taking notes from doctor visits, filing insurance claims, and offering basic triage.
Analytics Vidhya
His argument is that these same capabilities must be pointed at the bottom of the pyramid, not just at productivity gains in rich health systems.
AI as the “First Mile” of Care
In most advanced economies, the debate around AI in healthcare focuses on augmenting existing workflows: radiology, pathology, clinical documentation, and hospital operations. In the Gates framing, those use cases matter – but the most transformative opportunity is at the first mile of care: the moment when a person decides whether to seek help, where to go, and how quickly.
An AI-enabled first-mile stack in low-resource settings could include:
Symptom-checking and triage
A conversational agent that can ask structured questions, look for red-flag combinations of symptoms, and recommend urgency levels.
Decision support for community health workers
In many countries, the backbone of the health system is not doctors but community health workers with minimal formal training. AI tools could help them follow evidence-based protocols, avoid missed diagnoses, and know when to escalate.
Digital navigation of fragmented systems
AI systems could help patients understand which clinic has vaccines in stock, which hospital has an available bed, or whether a specific lab test is available locally.
- Anadolu Ajansı
- +1
- Diagnostics
- Discovery
- the Alzheimer’s Example
Gates’s AI agenda in health goes beyond frontline care. He has supported AI-focused challenges and funding rounds for diseases like Alzheimer’s, where traditional research has been painfully slow and expensive. One recent initiative offered a million-dollar prize pool for AI approaches that can accelerate Alzheimer’s research.
Instagram
In general, AI enables three high-impact diagnostic and research domains:
Imaging and pattern recognition
Deep learning models can outperform or match human specialists in interpreting X-rays, CT scans, and retinal images for conditions ranging from tuberculosis to diabetic retinopathy.
Pathology and genomics
AI tools can sift through digital pathology slides and genomic data to identify disease signatures, predict treatment responses, and guide precision medicine.
Drug repurposing and discovery
With large multimodal datasets, AI systems can suggest which existing drugs might be effective against new diseases, model protein interactions, and prioritize candidates for trials.
For low-income countries, the immediate relevance is not cutting-edge genomics, but the possibility of deploying AI-enabled diagnostic tools on low-cost hardware – for example, smartphone-based imaging kits combined with offline models for tuberculosis screening.
Health Economics: The 100-Dollar System
One of the most striking claims in Gates’s Doha remarks is that building an effective health system in poor countries could cost at most about 100 dollars per person per year.
Anadolu Ajansı
+1
That figure is not about funding highly specialized tertiary hospitals; it is about providing a baseline of:
primary care clinics,
vaccination programs,
maternal and newborn care,
basic diagnostics and essential medicines,
plus the digital and logistical infrastructure to support them.
AI does not magically generate that money. Instead, it changes two critical ratios:
Cost per unit of expertise delivered
If an AI system enables one doctor or nurse to safely support far more patients, the effective cost of expertise drops.
Cost of uncertainty
Better triage and early detection can prevent expensive complications and hospitalizations, freeing scarce funds for more coverage.
- Anadolu Ajansı
- +1
The Regulatory and Ethical Tightrope

It is important to note that Gates’s enthusiasm for AI in health exists alongside growing regulatory concern, especially in Europe. The European Commission has repeatedly signaled its intention to tightly regulate AI use in sensitive domains like healthcare, focusing on safety, transparency, and accountability.
Anadolu Ajansı
This tension is not accidental:
Under-regulation risks exposing vulnerable populations to unsafe or biased systems, misdiagnoses, and exploitation of health data.
Over-regulation risks locking out precisely the kind of experimentation and low-cost innovation that low-income countries need most.
- For Gates
- who has spent decades in global health philanthropy
- the key is trustworthy AI: systems that are validated
- monitored
- transparent about their limitations
- deployed through existing health infrastructure rather than in parallel to it.
The Risk of a New Digital Health Divide
Beneath the optimistic narrative lies a real danger: that AI could actually widen global health inequality.
- Wealthy countries could deploy AI tools to cut waiting times
- personalize treatments
- automate administration – further improving outcomes.
- Poor countries
- lacking data infrastructure
- connectivity
- local talent
- might see only a trickle of these gains
- or receive low-quality “stripped-down” tools.
- Anadolu Ajansı
- +2
- Yandex
- +2
But closing the gap will require:
- investment in digital public goods
- such as open-source models and reference datasets relevant to malaria
- tuberculosis
- maternal health
- other priority areas;
- capacity-building for local engineers
- clinicians
- regulators;
and governance frameworks that protect citizens’ data without blocking innovation.
What Bill Gates Is Really Asking For
- gatesnotes.com
- +2
- Anadolu Ajansı
- +2
The world is at risk of losing hard-won progress against poverty and disease.
Today’s global health toolkit is not enough to counteract that trend under current funding and geopolitical constraints.
AI offers a once-per-generation opportunity to radically lower the cost of expertise, accelerate research, and make health systems far more effective – especially where doctors are scarce.
- Realizing that potential requires deliberate choices: funding
- regulation
- global cooperation
- a focus on the poorest.
In that sense, when Gates calls AI an “extraordinary turning point” for health, he is not simply predicting a technological inevitability. He is describing a fork in the road: either AI becomes another force that primarily benefits rich countries, or it becomes a genuine equalizer. The outcome is a policy and investment choice, not a law of nature.
Frequently Asked Questions
- Is Bill Gates saying AI will replace doctors?
- New York Post
- +1
- What does “extraordinary turning point” in health actually mean?
- Anadolu Ajansı
- +1
- Why is Gates focused on languages in Africa and Asia?
- Anadolu Ajansı
- +1
How soon could these AI health systems be deployed at scale?
Technically, many components already exist: triage chatbots, clinical decision support, imaging models, and telemedicine platforms. The bottlenecks are regulation, funding, telecom infrastructure, and integration into real health systems rather than pilot projects.
- What is the biggest risk of AI in healthcare from Gates’s perspective?
- TIME
- +1
Conclusion
Bill Gates’s Doha Forum speech is more than a tech optimism sound bite. It is a diagnosis of a fragile global health landscape – and a prescription that leans heavily on AI as an amplifier of human expertise, not a replacement for it.
If his vision is to materialize, three things must happen in parallel:
- Aggressive deployment of AI tools tuned for low-resource settings
- local languages
- primary care use cases.
- Renewed investment in basic health systems
- so that AI augments real clinics
- real workers
- real supply chains instead of existing as a disconnected app.
- Global governance and cooperation that keep AI safe
- trustworthy
- accessible to the people who need it most.
The “extraordinary turning point” Gates speaks of is not guaranteed. But for the first time, a convergence of AI capabilities, mobile connectivity, and decades of learning in global health makes it technically plausible to imagine a world where a child’s chance of surviving does not depend on the country they were born in.
Whether that possibility becomes reality will depend less on algorithms and more on political will, funding decisions, and how seriously leaders take the kind of warning Gates delivered in Doha.